1 Introduction to pathology of the eye
The eye is a complex, unique structure, and a thorough description of the anatomy and physiology of the eye is far beyond the scope of these notes. An excellent summary is available in Chapter 21, p. 1269-1282 of the reference textbook (Zachary and McGavin), and I strongly encourage you to read it. A PDF copy of the chapter is available in Moodle. It will help provide a solid foundation that will allow you to understand the development of ocular disease, rather than simply memorizing the steps and lesions involved.
It is important to understand that the eye is a unique, highly organized structure, and that disruptions to the delicate structures of the globe can have significant and severe consequences to the health of the eye and to vision. Furthermore, the globe is a closed system, often sparing it from systemic insult, but also depriving it of quick and efficient resolution from damaging events like inflammation or hemorrhage. Recall that, like the brain and the testes, the eye has a form of immune privilege. There are relatively few resident leukocytes, leading to a relative delay in the onset of inflammation. Regeneration and repair is similarly limited in comparison to other tissues. Finally, unlike the liver or other tissues were parenchymal cells can divide and regenerate functional organ mass following injury, the eye has very little regenerative potential. Thus, any damage is of consequence to the eye.
Most of what we will deal with in this section is the pathogenesis and theory of disease. Where possible, we will look at the gross correlates, but many of the conditions are better appreciated with an ophthalmological exam, requiring specialized tools and techniques. Microscopic images will be used to help reinforce concepts and provide a visual correlate to the theory.
What follows in this chapter is a minimal review of the basics of ocular anatomy as it relates to pathology, to help refresh your memory after having read the textbook. I’ve also put together a general Glossary to help keep track of all the terms that are unique to ocular pathology and ophthalmology, and which seem to make up a language of their own.
1.1 Ocular anatomy
A video explanation of the following is available here, and a schematic of the eye is show in Figure 1.1. The globe is surrounded by muscular tissue, eyelids, and a bony orbit. The globe itself is made up of three conceptual layers: the sclera, which is modified at its anterior end to become the cornea; the choroid, a portion of the vascular supply of the eye; and the retina, the light sensing interior layer. The choroid is continuous with the iris and ciliary body. The lens, a structure designed to refract light, is suspended by zonules originating from the ciliary body. These structures create several compartments within the eye: the anterior chamber, posterior chamber, and vitreous humour. Each of these structures is complex and reacts to injury and disease in somewhat different ways.
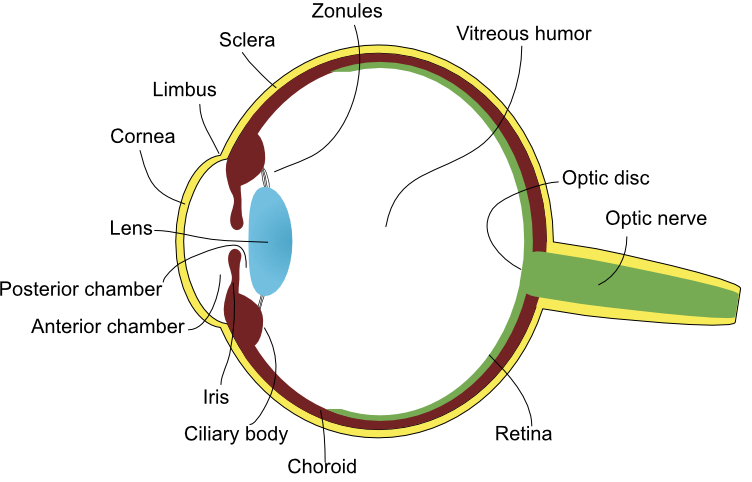
Figure 1.1: Cartoon of the globe illustrating many of the important anatomical structures. Note that the uvea is composed of the structures coloured red (the iris, ciliary body, and choroid).
The eyelids are covered on one side by haired skin, which is histologically similar to skin found in other areas. The other side is covered by conjunctival epithelium, known as the palpebral conjunctiva. Tear film, composed of mucous and fluid, is present between the bulbar and palpebral conjunctiva, and is distributed through the action of blinking. The eyelid margin is where the anterior haired surface and posterior palpebral conjunctiva meet. Cilia, or eyelashes, are present at the eyelid margin, along with a row modified sebaceous glands called meibomian or tarsal glands.
The eyelids help protect the eye from physical injury and help remove irritating contaminants from the surface of the eye. The tear film also contains antibacterial peptides. The eyelids respond to injury in much the same way as skin elsewhere in the body responds to injury. Given their role in keeping the eye protected and moist, however, damage resulting in defective function or congenital malformations (for example, Entropion and ectropion) can have significant consequences to the eye.
The conjunctiva is a mucous membrane that extends from the eyelid margin, spreads across the inner surface of the eyelid, and along the scleral surface up until the cornea. It is composed of stratified squamous, non-keratinizing epithelium, with goblet cells scattered throughout the palpebral, but not bulbar, conjunctiva. It is vascularized and innervated.
The sclera forms the bulk of the outer portion of the globe, and is readily identified as the thick, white, fibrous portion of the eye. Continuous with the sclera is the cornea, the clear, slightly bulbous portion of the eye through which light enters. The junction of the cornea and sclera is termed the limbus.
The cornea is a highly specialized piece of tissue and is formed by a unique arrangement of fibrous connective tissue that allows light to pass through. The cornea is composed of four layers: the corneal epithelium, the corneal stroma, Descemet’s membrane, and the corneal endothelium. The corneal epithelium, which is stratified squamous, lacks both pigment and keratin, and is replaced frequently – approximately once every 5 - 7 days. The corneal stroma is composed of thin, compact collagen fibrils arranged in parallel and separated by a space that corresponds to the wavelength of light, all of which serve to minimize the scatter of light. Importantly, the corneal stroma is maintained in a dehydrated state, through passive and active means. Within the corneal endothelium are energy-dependent sodium-pumps that remove solutes from the corneal stroma, creating an osmotic gradient that allows fluid to exit the stroma. To prevent the entry of fluid, the corneal epi- and endothelium are both maintained by tight intra-cellular junctions. Fluid within the corneal stroma is a common pathological finding in diseased eyes, and manifests as corneal cloudiness, often with a slight blue tinge.
The cornea is avascular, and therefore must rely on passive diffusion of nutrients and oxygen from conjunctival and scleral blood vessels, as well as from the tear film and aqueous humour. The presence of blood vessels within the cornea is a sign of pathology, either past or present.
The uvea is composed of three strucutres: the iris and ciliary body, which form the anterior uvea, and the choroid. The uvea is the vascular supply to the eye. The iris is composed of an innervated fibrovascular stroma with varying numbers of melanocytes. Two smooth muscles course through the iris, allowing it to change size and moderate the amount of light passing through the lens and onto the retina. The ciliary body is a small structure that extends from the posterior aspect of the base of the iris to the choroid. An important role of the ciliary body is the production of aqueous humour. It also serves to anchor the lens in place via thin, strong cables known as zonular fibers. The choroid supplies nutrients and oxygen to the posterior segment of the eye, most notably to the retina.
The lens refracts light to provide focus, and can change shape slightly depending on the tension applied to the suspending zonular fibers. A more detailed description is found in the section on the Pathology of the lens.
Finally, the retina is the nervous component of the eye, converting light to nervous impulse. The retina is a complex anatomical and physiological structure, and is discussed in more detail in the section on the Pathology of the retina.
1.2 Submitting a globe for histopathology
During the course of your clinical career, you will undoubetdly perform several enucleations, and hopefully you will submit the samples to your local pathologist. Putting the globe directly in formalin will usually provide adequate results, however, it takes awhile for formalin to perfuse into the eye and fix the retina, leading to the introduction of possible artifact. To avoid this, inject a small amount of formalin into the vitreous of the eye. Use a small gauge needle (25 g or higher), and pierce the globe at an angle. A good place to inject is immediately adjacent to the optic nerve (Figure 1.2). For small animals, about 0.5 ml of formalin is adequate; for larger animals, up to 1 ml may be required. The globe will fill noticeably taught following the injection.
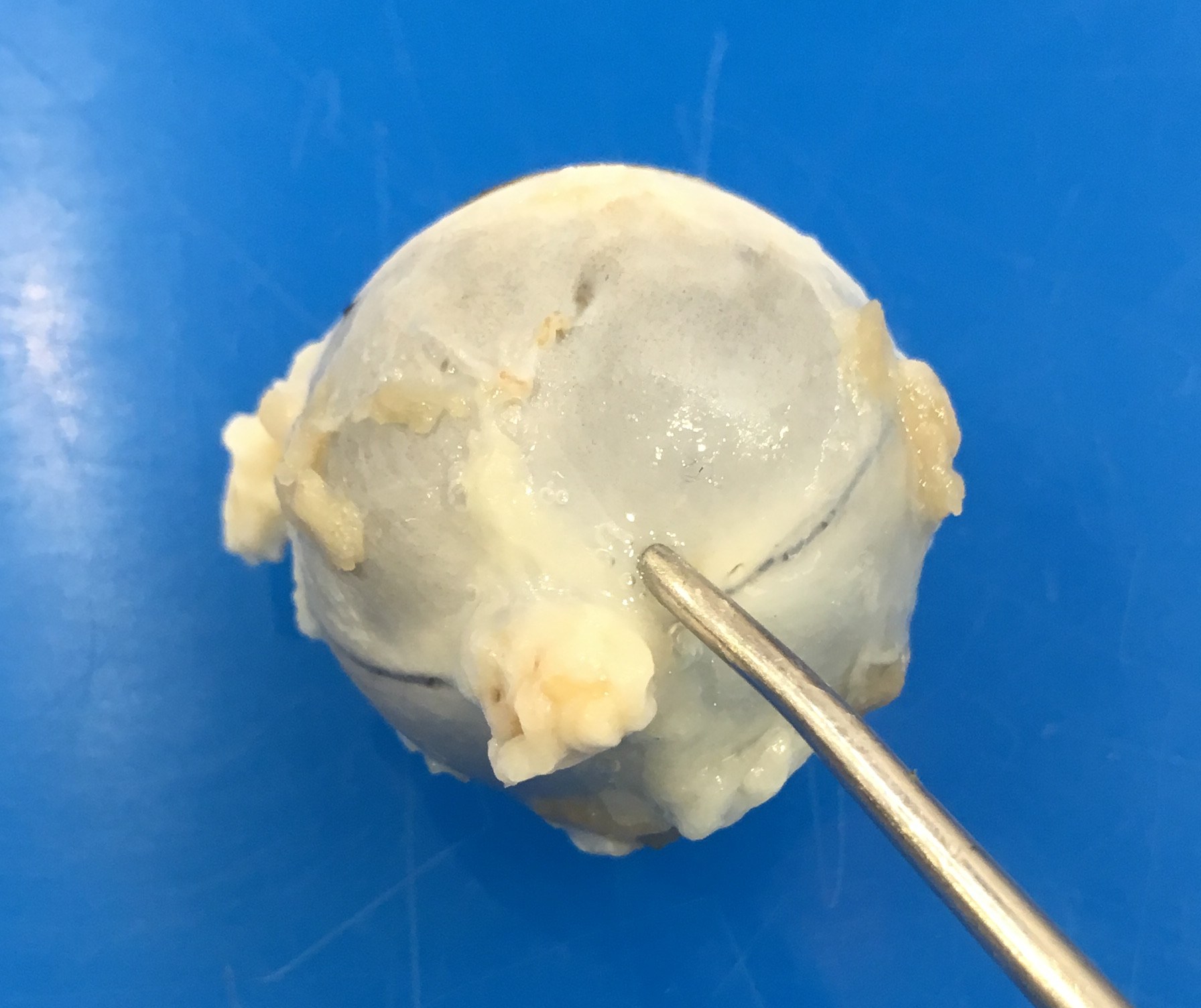
Figure 1.2: Landmarks for injecting the globe with formalin. You are viewing the caudal aspect of the globe. The probe (representing an ideal location to inject formalin) is at the caudal aspect of the eye, and just slightly dorsal.
Always remember to include a detailed and succinct history. Many of the eyes that are submitted for pathology are at a similar “end-stage”, and determining the underlying etiology is often impossible based on histopathology alone. The more information you provide, the more information the pathologist can then provide back to you. Don’t forget to include the duration of the clinical signs, treatments administered, and your differential diagnoses.